Legitimizing Instrument Adjusting
 Sunday, April 1, 2012 at 4:36PM
Sunday, April 1, 2012 at 4:36PM  Christopher J. Colloca, D.C.
Christopher J. Colloca, D.C.
CEO and Founder of Neuromechanical Innovations
A ISO 13485 Certified Medical Device manufacturer of the Impulse® family of adjusting instruments, based in Chandler, Arizona.
INTRODUCTION
As the popularity and utilization of Instrument Adjusting grows worldwide, mainstream acceptance continues to be hampered by outdated technology and technique approaches that are associated with traditional Instrument Adjusting techniques. The exciting challenges of integrating chiropractic care into mainstream healthcare are subsequently plagued by the esoteric chiropractic techniques that are not accepted or recognized among general healthcare professionals. Take for example, the Activator Method, which advocates that changes in leg length while a patient places their hand on their lower back constitutes a positive clinical finding for an L5 or L4 vertebral subluxation. Try explaining this test to a physician or even a chiropractic colleague!
Recently claims submitted to Aetna by Activator practitioners have been denied simply based upon the technique used. There is also the problem of using the Activator Method isolation tests to identify a subluxation under Medicare. So, while the Activator group should be congratulated for celebrating their 45th Anniversary in business, their decades old approach doesn’t pass the sniff test in today’s healthcare arena.
Recognizing the inherent dangers in being associated with other Instrument Adjusting approaches, our team set out to carve our mission of legitimizing Instrument Adjusting not only within chiropractic, but also to the general health care community and to the public. To this extent, our team crafted a strategic plan to assess instrument adjusting utilization and perception and to provide the improvements and enhancements necessary to advance the technique and the profession.
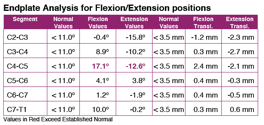
Instrument delivered chiropractic care can be broken down into two parts – The instrument technology itself and the clinical application that the technique is based upon (Figure 1).
 Figure 1. Instrument Adjusting includes the technology of the product represented by the instrument brand and the functionality or performance of the device as well as the clinical application that is taught in the clinical training that includes the indications to administer the treatment and the clinical decision making accompanying the actual technique application.
Figure 1. Instrument Adjusting includes the technology of the product represented by the instrument brand and the functionality or performance of the device as well as the clinical application that is taught in the clinical training that includes the indications to administer the treatment and the clinical decision making accompanying the actual technique application.
First level strategic inputs to assess in legitimizing Instrument Adjusting include Technology development and evaluation of the Clinical Applications. As shown in Figure 2, these inputs are driven by research and development resulting in scientific journal publications that validate the technology that is developed. Medical Device Certifications ensure quality and further solidify the medicolegal ramifications of using instrument adjusting technology in your practice. Through literature review, evidence-based Technique Development comprised the incorporation of clinical tests with the best evidence as inclusion criteria, and Clinical Training and practical testing to ensure clinical proficiency. Last, efforts to increase the awareness of the Instrument Adjusting movement within chiropractic were created through a Marketing and Business Expansion effort to increase the utilization of chiropractic care by the public.
 Figure 2. Categorization of the strategic input drivers identified to legitimize Instrument Adjusting.
Figure 2. Categorization of the strategic input drivers identified to legitimize Instrument Adjusting.
- Technology Inputs
Instead of starting with an instrument and then doing retrospective research the way instrument adjusting research has traditionally been approached, we set out to prospectively develop a new family of adjusting instruments to improve the performance and efficiency of chiropractic adjustments. The Impulse® and Impulse iQ® Adjusting Instruments were born of this research.
We quantified the forces and speeds that were necessary to maximize vertebral motions and neuromuscular responses (1,2) and investigated how instrument delivered thrusts differed among normal and pathological states such as disc degeneration and muscle hyperactivity (2-4). We then compared our new technology to existing adjusting instruments in the market and demonstrated the superiority of the biomechanical characteristics of the new Impulse® Adjusting Instruments (5,6). Validation of a new non-invasive method of dynamic spinal stiffness assessment was conducted and published it in the Journal Spine (7).
- Medical Device Certifications.
To meet the growing demand for our products, I began a new medical device manufacturing company to manufacture the devices to the required specifications. We created several new jobs and instituted a Quality Management System to drive our business that fostered our ISO 13485 Medical Device Certification. Independent audits conducted in our facility ensure the safety and efficiency of our systems and procedures and our products UL Listing® attests to the high standards we hold. Our international growth pushed us to receive our Class II Medical Device Certifications throughout the World. Manufacturing a chiropractic device to the highest quality medical standards allows our equipment to be used in hospitals as well as private chiropractic clinics further serving the purpose to legitimize instrument adjusting.
- The Instrument Adjusting Problem - Esoteric Techniques
Unfortunately however, Instrument Adjusting has been traditionally associated with esoteric chiropractic analyses that border on summoning the supernatural. Followers of the Activator Method stare at the feet looking for leg lengths to change while asking the patient to put their arms on their back or over their head to confirm a vertebral subluxation at a specified level. Without any validation whatsoever, these arm movement are assigned to a particular vertebral segment and flexing the legs supposedly tells the clinician what side to adjust the patient on. Borrowed and adapted from Directional Non-Force Technique (DNFT), Activator technique is closer to Network and Applied Kinesiology with its leg checks, pressure tests and challenges that are seen by many as nothing short of strange and indefensible.
Without any credible explanation or rationale at all behind this analysis, the Activator Method is taught in our chiropractic colleges and in college sponsored post-graduate education courses. There aren’t too many chiropractic techniques that could be more far-fetched; yet, Activator Methods boasts that approximately 150,000 chiropractors have been trained in the technique. It’s hard to understand how this is even possible when there are approximately 50,000 chiropractors practicing in the USA and 90,000 abroad (8). Another descendant of DNFT, Koren Specific Technique, advocates that you can “adjust disks … see dramatic retracting … and specifically analyze and adjust yourself.” Rather than passing judgment, let’s have you decide for yourself what type of Instrument and technique method that you would like to subscribe. At the very least, I think you can understand why I felt the need to legitimize instrument adjusting.
- Clinical Application Inputs
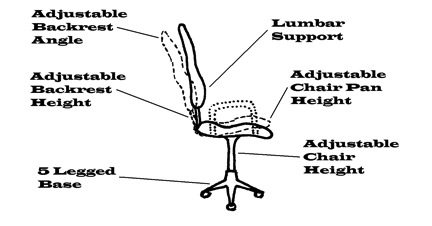
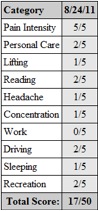
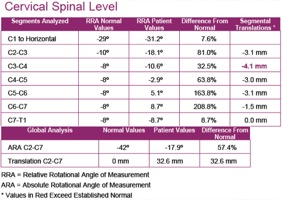
In developing Impulse Adjusting Technique (the clinical application training accompanying our products), we knew that we needed to incorporate logical, clear and readily acceptable objective assessments that were validated, accepted, and easy to perform. We embraced the Centers for Medicare (CMS) Services mandated P.A.R.T. analysis to keep chiropractors in compliance with regulations and increase their reimbursements at the same time. Incorporating accepted orthopedic tests combined with static palpation, and range of motion assessment of the spine and extremities, Impulse Adjusting Technique® considers the patients response in terms of their pain response (P), asymmetries (A), restrictions in range of motion (R) and the texture and tone changes in the muscles (T) as clinical indicators. With this approach, the most valid clinical indicators are incorporated and a straightforward patient encounter on each visit can subjectively and objectively track patients’ progress consistent with the chiropractic standard of care.
Clinical training in the Impulse Adjusting System® is offered in most U.S. Cities and many international destinations. Didactic and practical sessions are offered in the proper product usage and clinical applications training. A written and practical certification examination is offered to measure student’s proficiency. We have further developed a business and marketing expansion module to assist chiropractors in promoting and marketing their unique niche in chiropractic practice. More information can be found online at www.impulseseminars.com.
Legitimizing instrument adjusting and advancing the chiropractic profession begin with raising the standards of the products offered to DC’s replacing nonsensical chiropractic analyses with those techniques that have stood up to the scrutiny of research.
References
 CBP Seminars | Comments Off |
CBP Seminars | Comments Off |